Nearterm Blog
CMS to Reimburse Physicians Despite ICD-10 Coding Mistakes
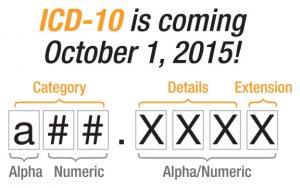
The CMS has made a concession in the transition from ICD-9 to ICD-10 that allows for reimbursement despite ICD-10 coding mistakes in claims, so as long as the physician used a valid code from the right family. This allows for flexibility in the claims auditing and quality reporting process and allows reimbursement to be made as the medical community gains experience using the new ICD- 10 code set. This is good news for providers as timely reimbursement of claims is critical for revenues cycle management. Learn more about what healthcare revenue cycle management companies can offer.
The exact words from a joint CMS and AMA Announcement:
“While diagnosis coding to the correct level of specificity is the goal for all claims, for 12 months after ICD-10 implementation, Medicare review contractors will not deny physician or other practitioner claims billed under the Part B physician fee schedule through either automated medical review or complex medical record review based solely on the specificity of the ICD-10 diagnosis code as long as the physician/practitioner used a valid code from the right family.”
For a political perspective, see: CMS will reimburse ICD-10 mistakes for one year after transition deadline.
Also from a CMS news release:
“With less than three months remaining until the nation switches from ICD-9 to ICD-10 coding for medical diagnoses and inpatient hospital procedures, The Centers for Medicare & Medicaid Services (CMS) and the American Medical Association (AMA) are announcing efforts to continue to help physicians get ready ahead of the October 1 deadline.”
The efforts to help physicians include:
- The “Road to 10” website to help with implementation that includes a countdown clock and primers for clinical documentation, clinical scenarios and other specialty-specific resources.
- Provider training videos that offer helpful ICD-10 implementation tips.
- Also, at the request of the AMA, a CMS ICD-10 Ombudsman (yet to be named) is to be appointed to triage and answer questions about the submission of claims. The ICD-10 Ombudsman will be located at CMS’s ICD-10 Coordination Center.”
Need help with ICD-10 Coding or implementation assistance? Want to learn more about your electronic claims submission clearinghouse options?
Nearterm offers interim or co-sourced, on-site or remote certified medical coders. Download: Certified HIM/Medical Coders: Remote or On-Site PDF